Temporomandibular Joint Diseases
Everything you need to knowTemporomandibular Joint Diseases
Jaw joint surgery, Jaw joint anatomy, Loss of mouth opening, Jaw dislocation, Jaw joint dysfunction, Jaw joint surgery process, Jaw joint prosthesis
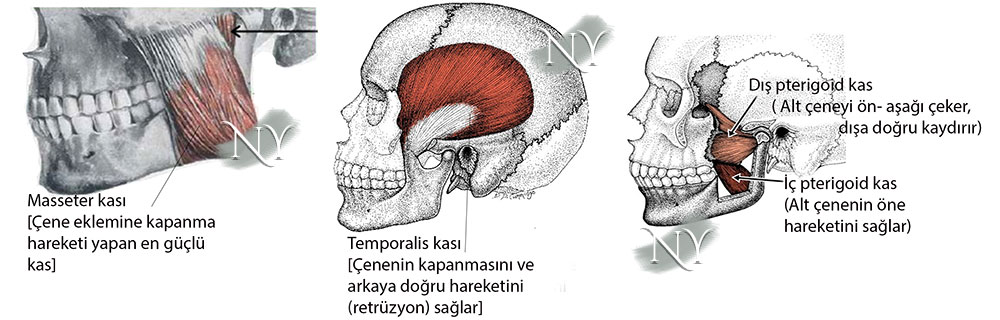
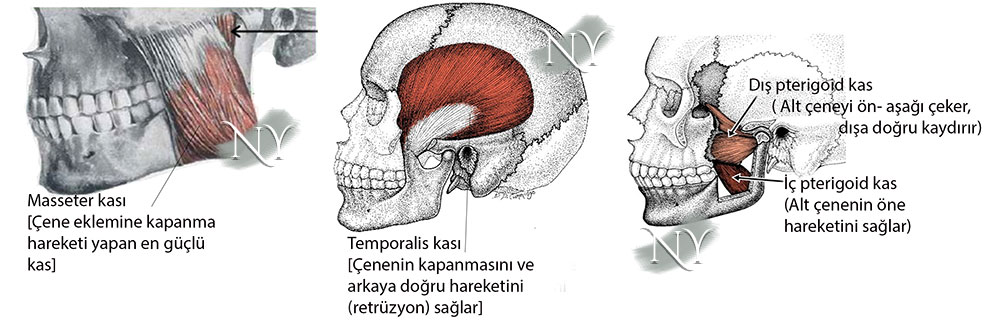
The jaw joint (temporomandibular joint), which is one of the most mobile joints in the body, consists of the condylar protrusion of the lower jaw bone, the articular surface of the temporal bone, articular cartilage, articular disc, ligaments surrounding the joint and muscles that provide movement.
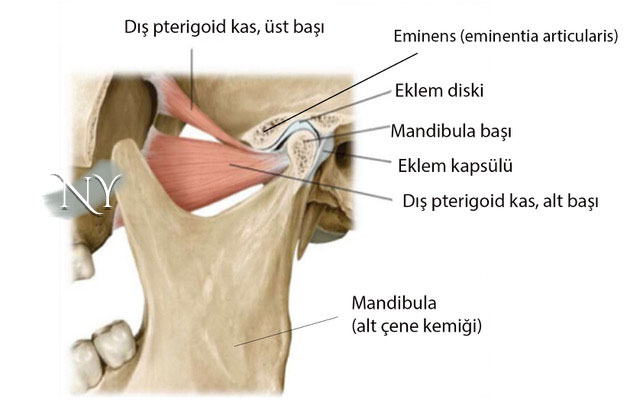
Image note: Jaw joint anatomy
Jaw joint disorders can be observed at a rate of up to 30% in society, being more common in industrial societies. The main reasons for this are;
- Teeth clenching and grinding due to depressive problems,
- Bite disorders due to dental disorders,
- Impacted teeth disrupt the biomechanical balance of the joint
- Inflammatory conditions due to blow to the jaw
- It can be listed as muscle spasm.
There are 4 basic muscles that move the jaw joint, and these muscles work in balance to move the lower jawbone forward, backward and sideways, allowing food to be crushed.
The jaw joint has a very durable infrastructure. The main muscle elements that perform the function in this joint, which is located within an armor consisting of joint ligaments and joint capsule, are the temporal muscle, which is the strongest masticatory muscle, and the external and internal pterygoid muscles, which are auxiliary muscles, and the muscles called masseters .
Spasm of the internal pterygoid muscle, one of these muscles, causes the mouth to be unable to open (trismus).
Although jaw joint dysfunction occurs in various forms, insufficiency in mouth opening is the most valid finding to make this diagnosis.
Patients presenting with jaw joint disease present with pain in the joint, a crunching sound, the joint coming out and falling into place, and a decrease in mouth opening. The reason for this is basically the disorders that occur in the joint cavity and joint disc. In any case, jaw joint dysfunction can be mentioned in patients with a mouth opening of less than 3.5 cm.
If the patient previously had rheumatic joint disease (such as rheumatoid arthritis), there may also be a significant decrease in mouth opening in the morning. This condition, which we define as joint stiffness, decreases throughout the day and mouth opening increases.
Up to 30% of the population experiences complaints suggestive of jaw joint problems at some point in their lives.
Among jaw joint diseases, in addition to loss of mouth opening due to problems in the joint disc, there is also a diagnosis called jaw dislocation.
Often, when mouth opening increases while yawning, the jaw joint may come out, usually downwards. In these patients, long-term and repeated jaw trauma (teeth clenching, grinding, etc.) is the main factor. In patients who develop jaw dislocation more than 3 times a year, surgical procedures to strengthen the jaw joint capsule are required. In cases where the jaw joint is dislocated, the joint is repositioned with special maneuvers. Before this, the patient is given muscle relaxants and sedatives to reduce the tension caused by the dislocation. I recommend patients an elastic bandage to the head area and various behavioral changes for at least 1 month afterwards.
In patients with jaw joint dysfunction, significant improvements can be achieved even with behavioral adjustments alone.
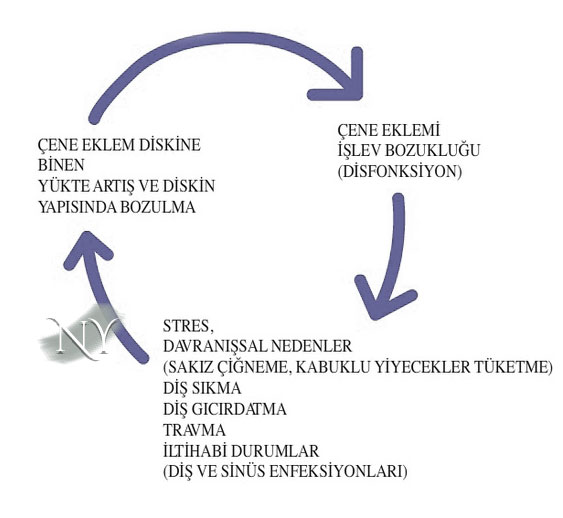
Jaw joint patients basically put long-term load on the jaw joint, causing joint deformation. This is a vicious circle and must be broken at some point.
For example, shelled foods should not be consumed, gum should not be chewed, patients who wear a headscarf should not hold the needle between their teeth while tying the headscarf, and if they have tooth decay or tooth alignment disorders, they should have it treated. Even in patients with a hunched posture, these problems may be encountered due to spasm in the jaw joint muscles due to vectorial effects. Therefore, our patients should not exhibit poor posture.
There are publications showing that various antidepressants are very effective in patients with complaints of teeth clenching or grinding at night (e.g. tricyclic antidepressants). For this reason, I recommend psychiatric support to patients with these complaints, even if they do not have depressive problems. Because some antidepressants are not only used in the treatment of depression.
Another joint-protective treatment for teeth grinding is intraoral dental splints. Splints are specially prepared by the dentist. It is possible for the person to get used to the splint with regular use for about a week. It may also be useful in the treatment of snoring.
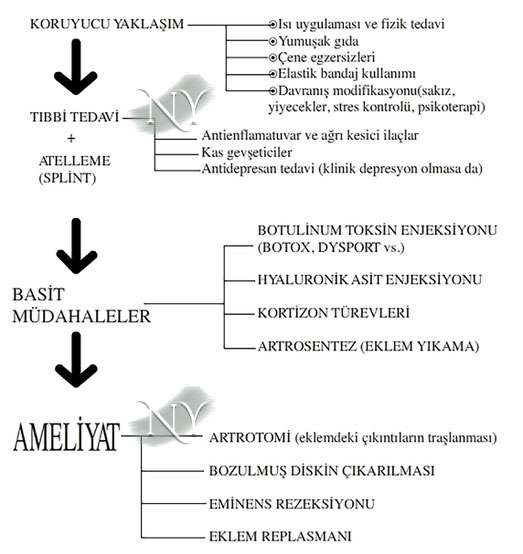
Jaw joint diseases require a stepwise treatment process. Unless the disorder is severe, I do not recommend that patients undergo surgery without going through these steps step by step.
Along with behavioral changes, I recommend physical therapy support (heat applications, jaw exercises, etc.) to my patients. Painkillers and muscle relaxants that reduce the inflammatory process are also significantly beneficial in patients who complain of a lot of pain. In fact, the use of a splint can reduce the patient's complaints to a certain point by resting the joint at night. In patients whose complaints do not subside despite these, injection-based interventions are applied before surgery. The most important of these are the washing process inside the joint called arthrocentesis and the artificial joint fluid injections (hyaluronic acid) applied together with it . In arthrocentesis, two separate needles are inserted into the joint in front of the ear. While the intravenous fluid is flushed with serum from one needle, the fluid is withdrawn from the other needle. It is thought that it cleans the calcification foci and inflammatory tissues that may be located within the joint. Artificial joint fluids based on hyaluronic acid (e.g. Ostenil, Synvisc, etc.) can provide relief to patients for 2*3 months. Since there will be returns afterwards, joint washing and fluid injections must be repeated. Although
physical therapists also recommend injections of a drug called cortisone , which has a stopping effect on the inflammatory process, I personally do not recommend it due to problems such as further degeneration in the joints, osteoporosis, and increases in blood sugar in the long term. Botulinum toxin type-A (Botox, Dysport, etc.)
injections , which are used in jaw joint diseases as well as in many problems in recent years, can reduce the activity of the jaw muscles, especially the masseter, and reduce the load on the joint. Although it is very effective in relieving joint complaints, especially in patients with muscle spasm, there may be loss of strength around the mouth and a smoother transition at the corner of the jaw due to the thinning of the masseter. In this last case, the person may have a condition called "long face".

Generally, long faces are more easily noticed in patients with angled jaw corners. However, patients are generally satisfied with this relieved chin corner.
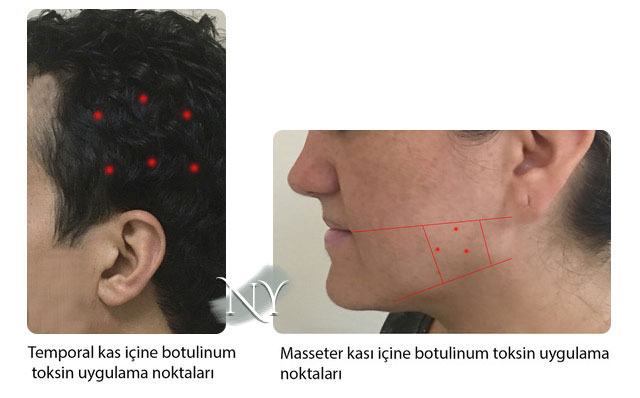
Botulinum toxin is a drug that works by causing decreased activity in the muscles, and the injection basically targets two separate muscles.
These are the masseter and temporal muscles. The effect of the injection lasts between 2-6 months, and in fact, additional injection in the middle of this period may be beneficial for the permanence of the effect.
Surgery is the last step in jaw joint dysfunction and the choice should be made according to the patient's complaint.
The surgery involves opening the jaw joint capsule and performing various procedures inside the joint. First of all, the most important risk of the surgery is the paralysis of the facial nerve , which passes through the adjacent area and distributes to the face . Paralysis of this nerve usually occurs not by cutting, but by pulling the soft tissues aside in order to see the joint clearly during surgery, and it usually resolves spontaneously within 1-3 months. I think I minimized this risk by approaching the joint from a slightly higher position than normal during the surgery. However, all of my patients take the risk of possible facial nerve paralysis when undergoing this surgery, and most of them are patients who have not been cured by other treatment steps.
Surgery may not provide a 100% solution, the basic expectations of patients are to ensure sufficient mouth opening, to eliminate abnormal movements and sounds in opening and closing the mouth, and to eliminate pain.
The main complaint of most patients is pain that has become unbearable. This pain is largely eliminated by cutting and burning the pain fibers that provide sensation to the joint during surgery. However, the vascular-nerve network behind the joint disc is another source of pain, and placing relaxing stitches on the joint disc to reduce the pressure in that area may be beneficial.
Another surgical solution is eminectomy, which involves shaving the bump in front of the joint called eminence. This process actually eliminates the joint and makes it flat, thus eliminating a friction point that would cause crunching when opening and closing the mouth. As long as the joint capsule is repaired properly, it does not cause any significant problems. I get satisfactory results from this surgery in most of my patients.
The condition of patients who experience intermittent dislocation in the joint is called habitual dislocation . In these patients, creating an additional armor surrounding the joint with the membrane layer (fascia) surrounding the temporalis muscle in order to strengthen the joint capsule generally reduces the complaints.
Joint prostheses are more problematic than thought in the long term and patients may require repeat surgeries. Since the surgical opening required to place the prosthesis is larger, the likelihood of injury to the facial nerve is higher.
Calcification in the joint , or ankylosis, is the most difficult to treat and most problematic disease of the jaw joint. Due to various reasons (trauma, rheumatic diseases, radiotherapy damage due to head and neck tumor, etc.), this calcification may cause the condylar protrusion of the lower jaw bone called the mandible to stick to the base of the skull.
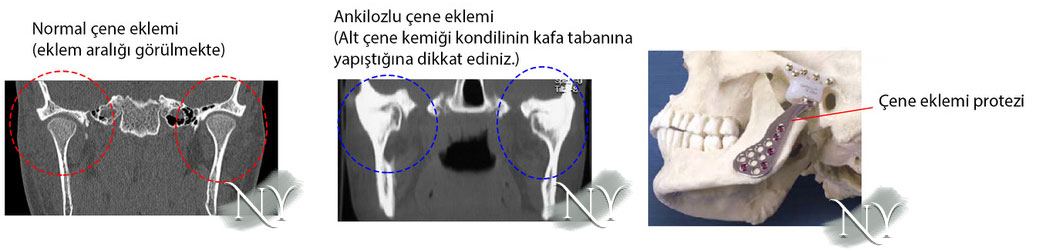 In such a case, it is generally recommended that the first stage of treatment is to open the adhesion by chipping the bone in surgery, to give movement to the joint, and then to create an artificial joint space by placing materials such as muscle membrane (fascia), tendon, and silicone block in between to prevent it from sticking again. This surgery, called gap arthroplasty , is the last exit point before joint prosthesis. However, no matter how well it is done, patients generally require either repeat surgery or treatment with joint prosthesis after 5 years.
In such a case, it is generally recommended that the first stage of treatment is to open the adhesion by chipping the bone in surgery, to give movement to the joint, and then to create an artificial joint space by placing materials such as muscle membrane (fascia), tendon, and silicone block in between to prevent it from sticking again. This surgery, called gap arthroplasty , is the last exit point before joint prosthesis. However, no matter how well it is done, patients generally require either repeat surgery or treatment with joint prosthesis after 5 years.
Joint prosthesis application is the last step of the treatment ladder in jaw joint dysfunction. The number of patients reaching this stage is a very small fraction when all jaw joint patients are considered. During the surgery, a larger incision is made and the side arms of the mandible bone are removed, including the calcified jaw joint area. This stage requires a lot of attention and serious bleeding may occur. Afterwards, the artificial prosthesis suitable for the patient's jawbone dimensions is fixed to the jawbone and the temporal bone, which will form the connection at the skull base, via titanium screws. The joint capsule is also repaired. After prosthesis surgery, the prosthesis may break due to situations such as loosening of the prosthesis or one or more of the screws being displaced. Therefore, patients with jaw joint ankylosis should know that they cannot use these joints as if they had never had the disease. The results promised by the joint can never be like the person's own natural jaw joint. With the latest technologies, personalized jaw joint prosthesis can be produced from three-dimensional printers and better results can be obtained mechanically.
"Health is the most important thing you have in life!"
Contact us now to schedule an appointment.