Impacted Tooth
Everything you need to knowImpacted Tooth
Impacted tooth extraction surgery is a surgery that is usually performed by putting the patient to sleep (general anesthesia). Teeth in proper position and orientation that are not fully embedded under the bone, but are only hidden under the intraoral covering called mucosa, may be preferred to be extracted with a nerve block.
Impacted (buried) teeth are teeth that emerge during the development process of the body, and while they may be useful in biting and chewing functions in some patients, they may develop poorly in others, harming oral and dental health and even general health.
Contrary to what our patients know , impacted teeth may not be located only in the upper or lower jaw (anatomical location) . There are cases of impacted teeth (ectopic impacted teeth) that have been observed to emerge in various parts of the body (in tumor formations such as paranasal sinuses, other skull bones, ovarian cysts or dermoid cysts) . Therefore, the interpretation and examination of a plastic surgeon is particularly important in determining the appropriate approach .

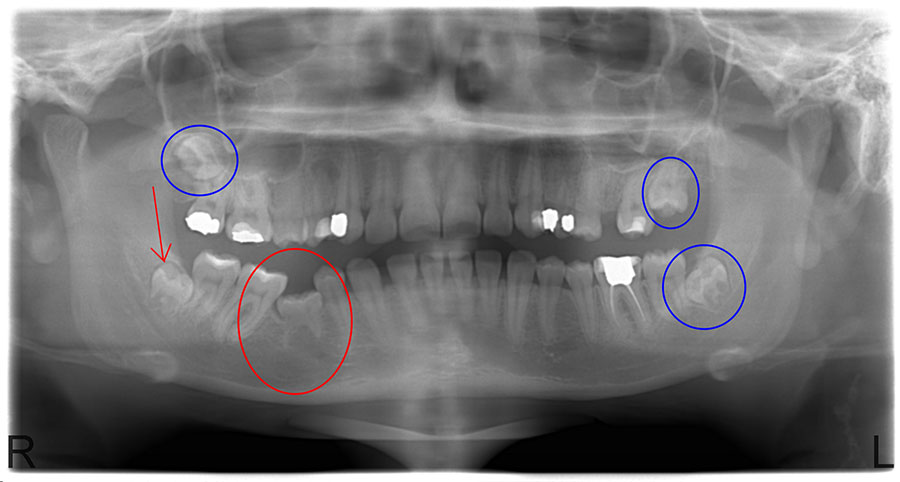
Image Note: Four embedded teeth stand out in the lower and upper jaw. Note that especially the ones in the lower jaw are now protruding from the bone.
Impacted teeth; In a study conducted by us, the most common complaints are pain in the jaw (92%), swelling in the cheek (79%), and impacted residual molar root due to previous extraction (16%) (1). Severe pain alone may be sufficient reason for tooth extraction. Apart from these, tooth root abscess, bone cysts, numbness in the lower lip, lower jaw fractures that occur with minor traumas, and jaw joint dislocations are also less common reasons for admission.
Although it is thought that impacted teeth occur due to disruptions in jaw and tooth development during the development process, various theories have been put forward on this issue.
According to orthodontic theory regarding the formation of impacted teeth ; Obstruction of the forward growth and eruption process in tooth and jaw development for any reason causes the teeth to remain impacted. According to another theory, Mendelian Theory ; In children whose jaw structure resembles the mother and the tooth structure resembles the father, as a result of a combination of genetic characteristics passed from parents to the child, the emergence of teeth may be prevented due to lack of space, especially if the mother's jaw is small and the father's tooth structure is large.
According to Phylogenetic Theory ; An important factor is the need for less chewing force due to the changing eating habits of people over the centuries, and the fact that the load on the bones is less, resulting in a smaller jaw structure in terms of volume compared to the past, and therefore the teeth in question cannot find space to grow. With the invention of fire, human beings began to eat meat by cooking it. and therefore the effectiveness of teeth in biting, tearing and crushing has also changed. Another dimension of the phylogenetic theory is that these embedded teeth are one of the organs that are used in other living species but cannot be used in humans. Just like the prematurely inflamed appendix vermiformis (as in appendicitis), some people are born with more than normal nipples along the trunk. Likewise, dermoid cyst-type tumoral formations may contain formations such as teeth and hairballs, which are actually examples of ectopic impacted teeth.
Impacted teeth; Although the above-mentioned theories have been put forward for the formation of teeth, what they have in common is either lack of space in the emergence of teeth or the presence of external factors that delay the development.
It is possible to summarize the pathological conditions that will lead to the presence of impacted teeth as follows;
- Systemic factors; These are diseases that concern the whole body. These diseases can occur either during the development process in the womb (prenatal) or after birth (postnatal). Related to the process in the womb are ancestral transmission, interracial marriages, the mother's faulty diet, and some infections experienced in the womb. Those that may occur during the postnatal development process are; Factors such as rickets, anemia, febrile diseases, trauma, and hormonal disorders can be listed.
- Regional factors; Regarding the tooth and the surrounding tissues, the following are the reasons why baby teeth do not fall out for a long time, long-term chronic inflammation, the bone on which the tooth sits does not develop adequately due to inflammatory diseases, the presence of infection or abscess around the tooth, and the pushing effect of adjacent teeth due to structural and alignment disorders.
- Congenital anomalies; In general, these are situations in which the tooth alignment may be distorted from the beginning. For example, in cleft palate, the tooth alignment is distorted, and since there is a cleft in the bone called alveolus, where the teeth are located, the tooth will not come out. On the other hand, problems may arise in the development of all teeth. Apart from this, impacted teeth may also be encountered in patients with deformities called craniosynostosis , which is due to premature fusion of the joints between the skull bones. Congenital metabolic diseases of the connective tissue ( such as achondroplasia ) can also negatively affect tooth eruption.
Impacted teeth differ structurally and it is important to plan extraction according to the neighboring structures around their location.
Impacted teeth located in the lower jaw usually show themselves in the 20s and are called wisdom teeth or wisdom teeth . Wisdom teeth do not always remain impacted. Properly growing ones can, in rare cases, adapt to the normal alignment adjacent to the second molar. However, they mostly tend to lean inwards, outwards, forwards and backwards. Teeth that are in a tilted position may need to be removed by opening a window in the bone, especially if they are embedded under the bone. During the extraction of lower jaw impacted teeth, it may be necessary to make some incisions in the oral covering.
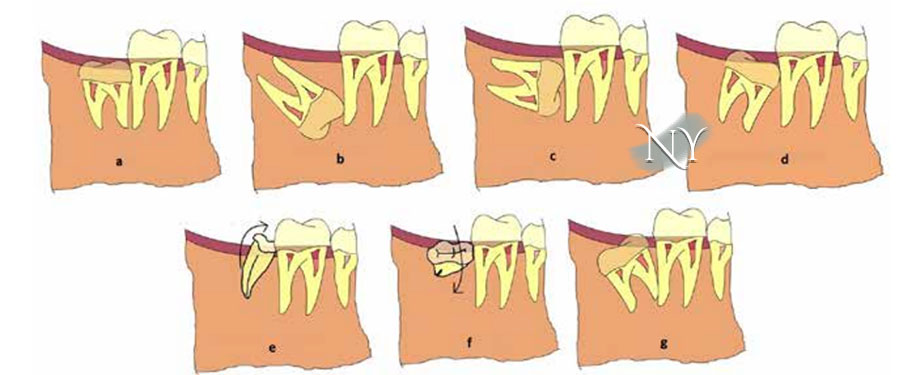
Image Note: Impacted teeth in the lower jaw may tend to lean in various directions. Surgical planning is different for each type.
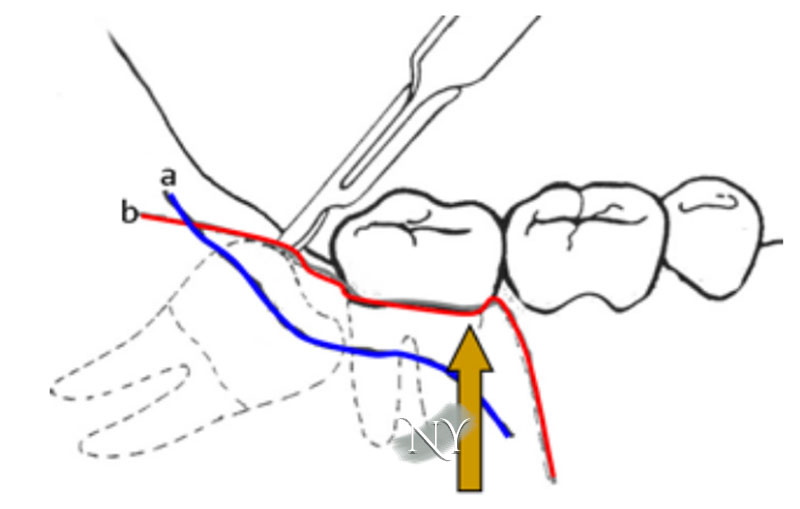
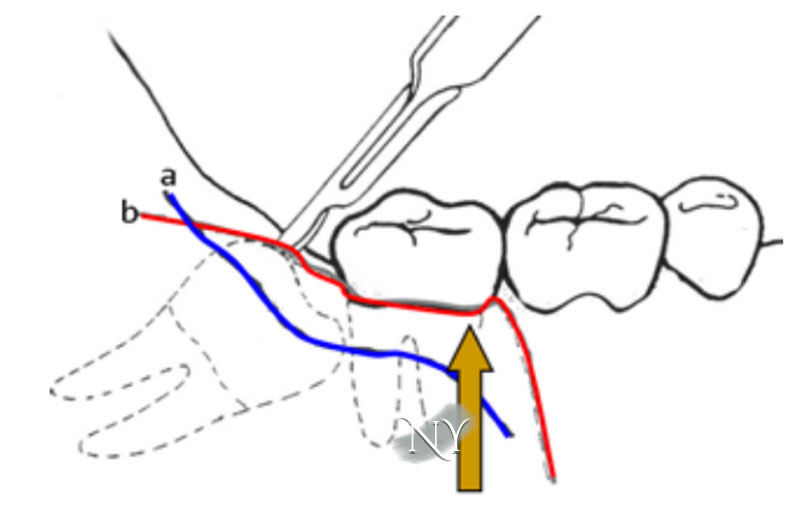
Image Note: Incisions used for molars that are located behind the second molar and are completely buried under the oral cavity. These do not leave any visible traces from the outside.
Impacted teeth may not always need to be extracted. A properly erupted impacted tooth can be preserved, especially if there is a corresponding bite point on the top.
Impacted teeth generally remain silent unless they manifest themselves with pain in the jaw. The cause of pain in the jaw is basically the impacted tooth pushing the others. In some patients, tooth axis distortions, which can be described as a tree blowing in the wind, may occur due to advanced diagnosis . Therefore, such tooth alignment disorders constitute a necessity for the extraction of the impacted tooth.
Impacted teeth, especially when located in the upper jaw, can cause frontal pain originating from the jaw joint. In this case, extracting these teeth may be beneficial to ensure the biomechanical balance of the jaw joint.
If the impacted tooth is in the lower jaw, it is located in the corner of the jaw and forms the weak point of the bone tissue here. Therefore, it paves the way for the lower jaw bone to break with minor impacts. In these patients, if the tooth prevents the bone from being placed on top of each other and there is a possibility of infection in the tooth socket, the tooth may need to be extracted.
Image Note: Two fully lying impacted teeth in the lower jaw. These are difficult to remove and require creating a window in the bone.
When wisdom teeth decay, they also require extraction. In such a case, it may be necessary to leave the tooth socket open and apply a dressing with antibiotic gauze. Decay of wisdom teeth can predispose to chronic sinusitis.
Impacted (bump) tooth surgery, as with all surgeries, involves a wound healing process and, in addition, a bone healing process. Therefore, my patients should consider some suggestions before these surgeries.
Impacted tooth surgery takes approximately 1 hour and can be performed by anesthetizing the patient (general anesthesia) or using regional anesthesia in the form of nerve blocks. Permanent numbness related to nerve blocks has been described in patients. For this reason, I generally recommend that the patient be anesthetized or the tooth be anesthetized locally. Things to consider after surgery can be summarized as follows:
- Smoking tends to impair wound healing and bone healing. Please stop smoking at least 1 week before surgery. Smoking may additionally increase the problems that general anesthesia may cause during surgery. Our patients who continue to smoke are deemed to have accepted these risks.
- Please take good basic oral and dental care until and after the surgery. Oral and dental care is very important for the wound and bone healing process. The most basic approaches for this purpose are to brush your teeth at least twice a day and use dental floss or dental interface brushes frequently.
- Impacted tooth extraction is a surgery, and in order to minimize the risks of this surgery, please give your doctor detailed information about your previous diseases and surgeries, regularly used medications, and any allergies you have. For example, your risk of bleeding during and after surgery may increase due to regular aspirin use. Again, this surgery requires protective (prophylactic) antibiotic injection before surgery, as it may increase your risk of cardiovascular system infection called bacterial endocarditis in patients with heart valve diseases. Do your research once again regarding the qualifications of people who do not try to get detailed information from you on this subject in terms of impacted tooth extraction.
- Mouthwashes should be used due to their antiseptic effect, especially the day before and on the day of surgery. In various clinical studies, it has been stated that the only effective mouthwash in this regard is chlorhexidine mouthwash. In addition, rinsing with salt or carbonated water may also be beneficial to speed up the healing process of the gums after surgery.
- Drug-resistant high fever (above 38.5 degrees Celsius) before the surgery, widespread swelling in the chin area, palpation of the lymph nodes under the chin indicate the presence of an abscess in your tooth that needs to be drained and, if necessary, hospitalized and treated with intravenous antibiotics. In this case, tooth extraction surgery should be postponed until the existing abscess is surgically opened and the clinical picture is corrected. However, if the tooth and its residues remain in the abscess formation during the surgery, it will be removed by curettage. As we have stated, with the application of intravenous antibiotics for at least 5 days (broad spectrum is started first and changed according to the results of the tissue culture taken during the surgery), a possible meningitis, brain Life-threatening problems such as abscess or bacterial endocarditis can be prevented.
Impacted tooth extraction surgery is a surgery that is usually performed by putting the patient to sleep (general anesthesia). Teeth in proper position and orientation that are not fully embedded under the bone, but are only hidden under the intraoral covering called mucosa, may be preferred to be extracted with a nerve block. However, in nerve blocks, very rarely the block is either permanent or can last for a very long time. In this case, the patient may experience the problem of not being able to feel one half of the lower lip (1-20).
During the extraction of the areas of the impacted teeth located under the bone, incisions are made in the intra-oral covering, which we call the mucosa, and the tissues are separated towards the edge, and the tooth is accessed by opening a window with special tools in the underlying jawbone. The ligaments around the tooth are loosened and the tooth is taken out. In case of poorly oriented teeth, it would be appropriate to cut the tooth into smaller pieces and remove it without damaging the neighboring teeth.
At the end of impacted tooth surgery, the opened mucosa tissue is closed with self-dissolving stitches. If there is tooth decay, it may sometimes be necessary to place a medicated gas tampon in the tooth socket and leave it open.
Image Note: It is possible for the lower right impacted molar (red arrow) to push the teeth in a way that prevents the eruption of the front molar (red circle) . Other impacted teeth (blue circles) also put pressure on neighboring tooth roots.
After impacted tooth surgery, your cheeks may swell and sometimes you may not be able to close your mouth unless you apply ice.
Impacted dental surgeries may not always yield positive results. Your positive results begin with the rapid disappearance of tooth-related pain from the first day and end with the reduction of swelling. In this process, you should pay attention to the following:
- The most common problem after impacted tooth surgery is swelling in the cheeks due to soft tissue edema. Applying ice for 15 minutes per hour during the period when the swelling is most intense for up to 1 week after the surgery will significantly reduce your complaints. There are also articles stating that eating ice cream is beneficial. As the number of teeth extracted increases, the amount of edema and swelling also increases. Ice application provides relief by reducing cheek edema very quickly.
- Do not smoke before or after the surgery . We recommend that our patients who require time do not drink at all during the first 6 weeks, during which the basic stages of bone healing are passed.
After impacted tooth surgery, use the medications and mouthwashes I recommend regularly until the oral lining (mucosa) heals. I also give information about how much medication our patients who have had heart valve disease will use during a face-to-face meeting.
After impacted tooth surgery, especially in patients with wisdom teeth extracted from the lower jaw corner, it is recommended that you do not eat shelled foods for the period recommended by your doctor. This is true even if you use the opposite side of your jaw. Remember that jaw fractures that may occur after lower jaw wisdom tooth extraction are more common than jaw fractures that may occur during surgery. In various publications, the first month on average has been reported as the most common period for such jaw fractures. Sudden pain, especially when eating something, accompanied by a crunching sound, may be signs of bone fracture.
After the surgery, you may observe clot accumulation under the gauze placed in your tooth socket for pressure purposes.
One of the most basic components of the healing process after impacted tooth surgery is clot formation. Especially the first stage of bone healing is clot accumulation in the damaged area. Please do not try to thoroughly clean this clot. Otherwise, the healing process may be negatively affected. Generally, if the tooth socket is not closed with stitches after extraction, we keep the placed gauze pad for a few hours. If you are not actively bleeding, the tampon can be removed.
Active, dripping or gushing bleeding within a few hours after impacted tooth surgery is not a normal finding. On the other hand, such bleeding is not expected in the days following the surgery. Therefore, our patients who experience such a problem should definitely inform their doctor. The reason for this may be a previously undetected and congenital bleeding-clotting disorder. In this case, the patient may need to be hospitalized again.
Resources:
- Khan I, Halli R, Gadre P, Gadre KS. Correlation of panoramic radiographs and spiral CT scan in the preoperative assessment of intimacy of the inferior alveolar canal to impacted mandibular third molars. J Craniofac Surg 2011; 22(2): 566-70. [CrossRef]
- Bodner L, Brennan PA, McLeod NM. Characteristics of iatrogenic mandibular fractures associated with tooth removal: review and analysis of 189 cases. Br J Oral Maxillofac Surg 2011; 49(7): 567-72. [CrossRef]
- Lim AA, Wong CW, Allen JC Jr. Maxillary third molar: patterns of impaction and their relationship to oroantral perforation. J Oral Maxillofac Surg 2012; 70(5): 1035-9. [CrossRef]
- Pell GJ, Gregory GT. Impacted mandibular third molars: classification and modified technique for removal. Dental Dig 1933; 39:330Y336.
- Almendros-Marqués N, Berini-Aytés L, Gay-Escoda C. Evaluation of intraexaminer and interexaminer agreement on classifying lower third molars according to the systems of Pell and Gregory and of Winter. J Oral Maxillofac Surg 2008; 66(5): 893-9. [CrossRef]
- Yeşiloğlu N, Temiz G, Sarici M, Filinte GT. A useful device for the improvement of maximal interincisor opening after operations of temporomandibular region: the clothes PEG. J Craniofac Surg 2013; 24(6): 2224-5. [CrossRef]
- Kriwalsky MS, Maurer P, Veras RB, Eckert AW, Schubert J. Risk factors for a bad split during sagittal split osteotomy. Br J Oral Maxillofac Surg 2008; 46(3): 177-9. [CrossRef]
- Pogrel MA. Permanent nerve damage from inferior alveolar nerve blocks: a current update. J Calif Dent Assoc 2012; 40(10): 795-7.
- Verma DK, Rajan R, Prabhu S. Ipsilateral, isolated amaurosis after inferior alveolar nerve block: report of two rare cases. Oral Maxillofac Surg 2013; 17(1): 73-5. [CrossRef]
- Yoon RK, Chussid S. Ocular complications following an inferior alveolar nerve block on a child patient: a review of the literature and report of a case. Pediatr Dent 2012; 34(4): 343-6.
- Tzermpos FH, Cocos A, Kleftogiannis M, Zarakas M, Iatrou I. Transient delayed facial nerve palsy after inferior alveolar nerve block anesthesia. Anesth Prog 2012; 59(1): 22-7. [CrossRef]
- Xu GZ, Yang C, Fan XD, Yu CQ, Cai XY, Wang Y, et al. Anatomic relationship between impacted third mandibular molar and the mandibular canal as the risk factor of inferior alveolar nerve injury. Br J Oral Maxillofac Surg 2013; 51(8):e215-9.
- Monaco G, Montevecchi M, Bonetti GA, Gatto MR, Checchi L. Reliability of panoramic radiography in evaluating the topographic relationship between the mandibular canal and impacted third molars. J Am Dent Assoc 2004; 135(3): 312-8. [CrossRef]
- Mercier P, Precious D. Risks and benefits of removal of impacted third molars. A critical review of literature. Int J Oral Maxillofac Surg 1992; 21(1): 17-27. [CrossRef]
- Wofford DT, Miller RI. Prospective study of dysesthesia following odontectomy of impacted mandibular third molars. J Oral Maxillofac Surg 1987; 45(1): 15-9. [CrossRef]
- Wagner KW, Otten JE, Schoen R, Schmelzeisen R. Pathological mandibular fractures following third molar removal. Int J Oral Maxillofac Surg 2005; 34(7): 722-6. [CrossRef]
- Werkmeister R, Fillies T, Joos U, Smolka K. Relationship between lower wisdom tooth position and cyst development, deep abscess formation and mandibular angle fracture. J Craniomaxillofac Surg 2005; 33(3): 164-8. [CrossRef]
- Ethunandan M, Shanahan D, Patel M. Iatrogenic mandibular fractures following removal of impacted third molars: an analysis of 130 cases. Br Dent J 2012; 212(4): 179-84. [CrossRef]
- Chrcanovic BR. Teeth in the line of mandibular fractures. Oral Maxillofac Surg 2014; 18(1): 7-24. [CrossRef]
- Shetty S, Angadi PV, Rekha K. Radicular cyst in deciduous maxillary molars: a rarity. Head Neck Pathol 2010; 4(1): 27-30. [CrossRef]
"Health is the most important thing you have in life!"
Contact us now to schedule an appointment.