Department Detail
Learn more about our departmentsOrthognathic surgery
Jaw joint surgery, Jaw joint anatomy, Loss of mouth opening, Jaw dislocation, Jaw joint dysfunction, Jaw joint surgery process, Jaw joint prosthesis
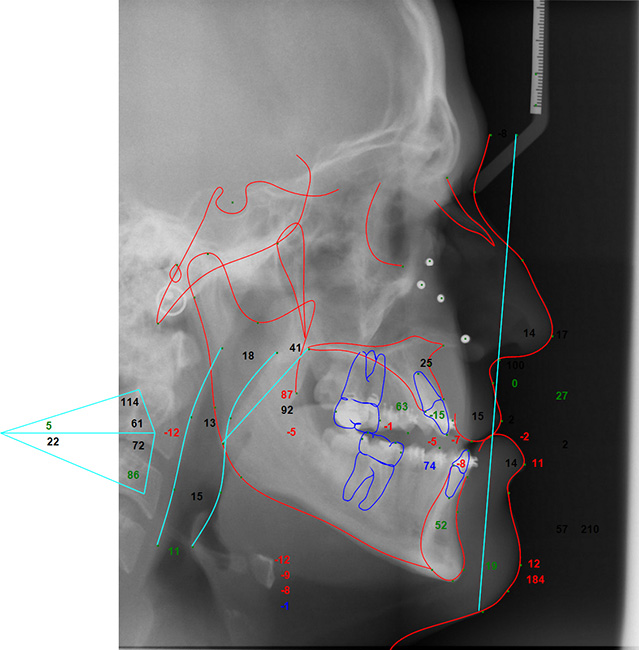
The jaw joint (temporomandibular joint), one of the most mobile joints in the body, consists of the condylar protrusion of the lower jaw bone, the articular surface of the temporal bone, articular cartilage, articular disc, ligaments surrounding the joint, and muscles that provide movement.
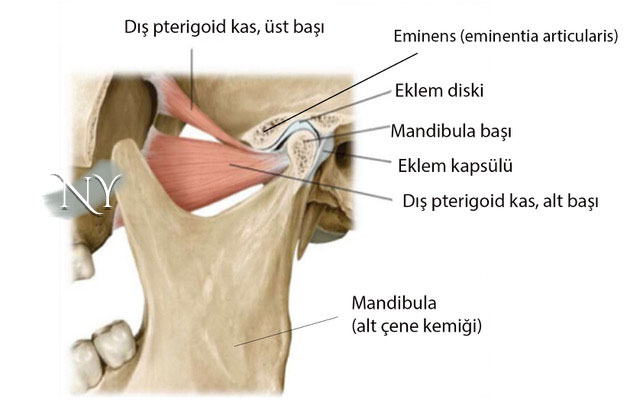
Image note: Jaw joint anatomy
Jaw joint disorders can be observed in up to 30% of the population, more so in industrial societies. The main reasons for this are;
- Clenching and grinding of teeth due to depressive problems,
- Bite disorders due to dental disorders,
- Impacted teeth disrupt the biomechanical balance of the joint
- Inflammatory conditions due to a blow to the jaw
- It can be listed as muscle spasm.
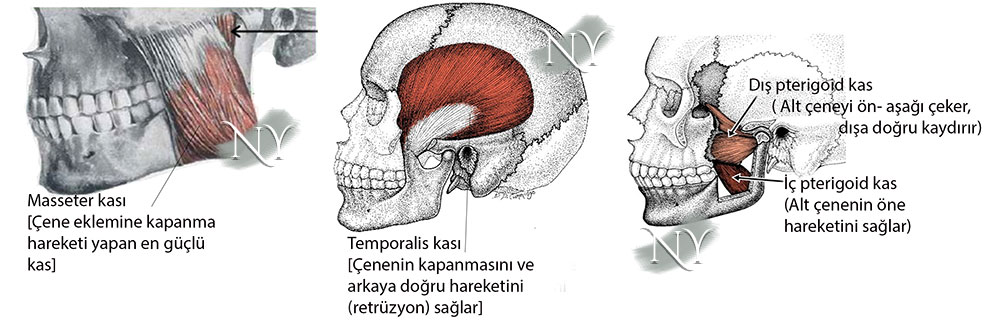
There are four basic muscles that move the jaw joint, and these muscles work in balance to enable the lower jaw bone to move forward, backward and sideways, thus crushing the food.
The jaw joint has a very durable substructure. The main muscle elements that perform the function in this joint, which is located in an armor consisting of joint ligaments and joint capsule, are the strongest chewing muscle, the temporal muscle , and the auxiliary muscles , the external and internal pterygoid muscles and the muscles called masseter .
Spasm of the internal pterygoid muscle of these muscles causes the mouth to not open (trismus).
Although temporomandibular joint dysfunction occurs in various forms, inadequate mouth opening is the most valid finding to make this diagnosis.
Patients presenting with jaw joint disorders present with pain in the joint, a crunching sound, the joint dislocating and settling into place, and decreased mouth opening. The main reason for this is the disorders that occur in the joint space and the joint disc. In patients with a mouth opening of less than 3.5 cm, in any case, jaw joint dysfunction can be mentioned.
If the patient has had rheumatoid joint disease before (such as rheumatoid arthritis), there may also be a significant decrease in mouth opening in the morning. This condition, which we define as joint stiffness, decreases during the day and mouth opening increases.
Up to 30% of the population experiences complaints that suggest a jaw joint problem at some point in their lives.
Among the jaw joint diseases, there is also a diagnosis called jaw dislocation, in addition to loss of mouth opening due to problems in the joint disc.
The jaw joint can usually dislocate downward and forward when the mouth is opened. In these patients, long-term and repeated jaw trauma (teeth clenching, grinding, etc.) is the main factor. In patients who develop jaw dislocation more than 3 times a year, it is necessary to perform procedures to strengthen the jaw joint capsule with surgery. In cases where the jaw joint is dislocated, the joint is put back into place with special maneuvers. Before this, the patient is given muscle relaxants and sedatives to reduce the tension created by the dislocation. Afterwards, I recommend an elastic bandage to the head area for at least 1 month and various behavioral changes.
In patients with dysfunction in the jaw joint, significant improvements can be achieved even with behavioral adjustments alone.
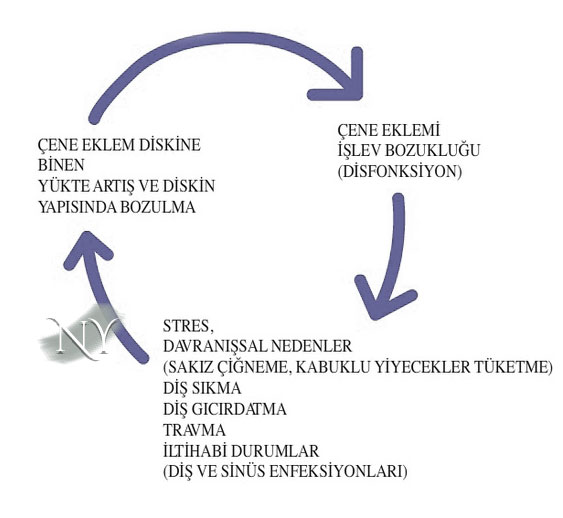
Jaw joint patients basically cause joint deformation by putting long-term load on the jaw joint. This is a vicious cycle and must be broken at some point.
For example, shellfish should not be consumed, gum should not be chewed, patients who wear headscarves should not hold the needle between their teeth when tying the headscarf, and if they have tooth decay or teeth alignment disorders, they should have them treated. Even in patients who have a stooped posture, these problems can be encountered due to spasm in the jaw joint muscles due to vectorial effects. Therefore, our patients should not exhibit posture disorders.
There are publications indicating that various antidepressants are quite effective in patients who complain of teeth grinding or clenching at night (e.g. tricyclic antidepressants). Therefore, I recommend psychiatric support to patients with these complaints, even if they do not have depression problems. Because some antidepressants are not used only in the treatment of depression.
Another joint-protective treatment for teeth grinding is intraoral dental splints. Splints are custom-made for the individual by the dentist. It is possible for the person to get used to the splint with regular use of about a week. It can also be useful in the treatment of snoring.
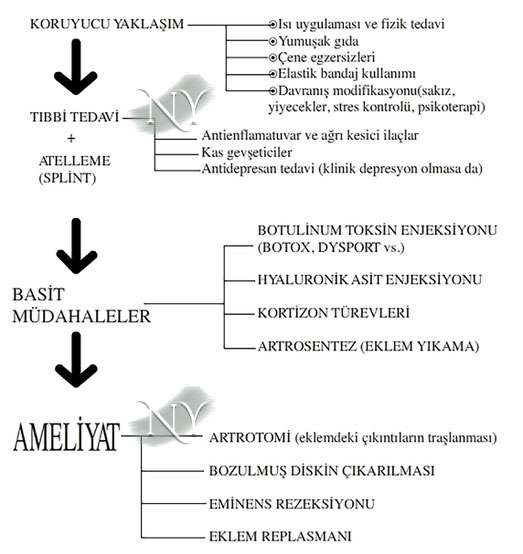
Temporomandibular joint disorders require a step-by-step treatment process. I definitely do not recommend that patients undergo surgery without going through these steps step by step, unless the disorder is severe.
Along with behavioral changes, I recommend physical therapy support (heat applications, jaw exercises, etc.) to my patients. In patients with severe pain complaints, painkillers and muscle relaxants that will reduce the inflammatory process are also significantly beneficial. In fact, the use of a splint can also reduce the patient's complaints to a certain point by resting the joint at night. In patients whose complaints do not improve despite these, injection-based interventions are applied before surgery. The most important of these is the joint washing process called arthrocentesis and the artificial joint fluid injections (hyaluronic acid) applied together with it . In arthrocentesis, two separate needles are inserted into the joint from in front of the ear. While the serum is washed with serum from one needle, the fluid is taken back from the other. It is thought that this cleans the calcification foci that may be located in the joint and the inflammatory tissues. Artificial joint fluids based on hyaluronic acid (e.g. Ostenil, Synvisc, etc.) can provide relief to patients for 2-3 months. Since there will be reactions afterwards, joint washing and fluid injections should be repeated.
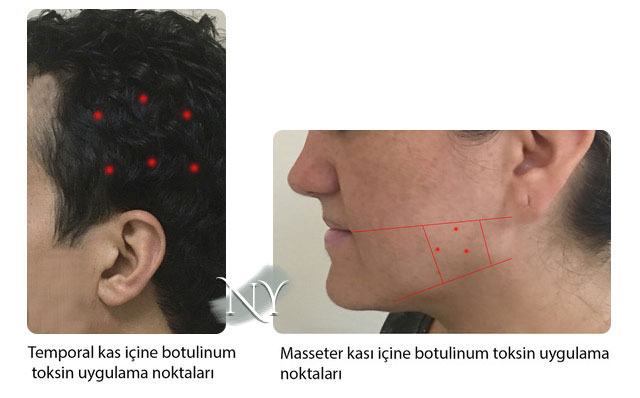
Physical therapists also recommend injections of a drug called cortisone , which has an effect of stopping the inflammatory process, but I personally do not recommend it because of problems such as more degeneration in the joint, osteoporosis, and increases in blood sugar in the long term. Botulinum toxin type-A (Botox, Dysport, etc.)
injections , which have been used in many problems in recent years as well as in jaw joint diseases, can reduce the activity of the jaw muscles, especially the masseter, and reduce the load on the joint. Although it is quite effective in eliminating joint complaints, especially in patients with muscle spasm, there may be loss of strength around the mouth and a smoother transition at the corner of the jaw due to the thinning of the masseter. In this last case, the person may have a condition called “long face”.

Generally, patients with an angled jaw have a longer face. However, patients are generally pleased with this relaxed jaw angle.
Botulinum toxin is a drug that works by causing a decrease in muscle activity, and the injection basically targets two separate muscles.
These are the masseter and temporal muscles. The effect of the injection lasts between 2-6 months, and in fact, an additional injection in the middle of this period may be beneficial for the permanence of the effect.
Surgery is the last step in jaw joint dysfunction and the choice should be made according to the patient's complaint.
The surgery involves opening the jaw joint capsule and various procedures inside the joint. First of all, the most important risk of the surgery is the paralysis of the facial nerve , which passes through the area adjacent to the area and spreads to the face . Paralysis of this nerve usually occurs not by cutting, but by pulling aside the soft tissues during the surgery to see the joint clearly, and usually resolves on its own in 1-3 months. I think I minimize this risk by approaching the joint from a slightly higher angle than normal. Nevertheless, all my patients take the risk of possible facial nerve paralysis into consideration when undergoing this surgery, and most of them are patients who have not been cured by other treatment steps.
Surgery may not provide a 100% solution; the basic expectations of patients are to ensure adequate mouth opening, to eliminate abnormal movements and sounds while opening and closing the mouth, and to eliminate pain.
The main complaint of most patients is the pain that has become unbearable. This pain is largely eliminated by cutting and burning the pain fibers that receive the sensation from the joint during surgery. However, the vascular-nerve network located behind the joint disc is another source of pain and placing relaxing stitches on the joint disc to reduce the pressure in that area may be beneficial.
Another surgical solution is eminectomy, which involves shaving the eminence, the bump in front of the joint. This procedure actually removes the joint and makes it flat, thus eliminating a friction point that would cause a crunch when opening and closing the mouth. As long as the joint capsule is repaired properly, it does not cause any significant problems. I get satisfactory results from this surgery in most of my patients.
The condition of patients with intermittent dislocations in the joint is called dislocation habit (habitual dislocation) . In order to strengthen the joint capsule in these patients, creating an additional armor surrounding the joint with the membrane layer (fascia) surrounding the temporal muscle generally reduces complaints.
Joint prostheses are more problematic than expected in the long term and may require repeat surgeries. The surgical opening required to insert the prosthesis is greater, so the possibility of facial nerve injury is higher.
Joint calcification , or ankylosis, is the most difficult to treat and most problematic disease of the jaw joint. Due to various reasons (trauma, rheumatic diseases, radiotherapy damage due to head and neck tumors, etc.), this calcification can cause the condyle protrusion of the lower jaw bone, called the mandible, to stick to the skull base.
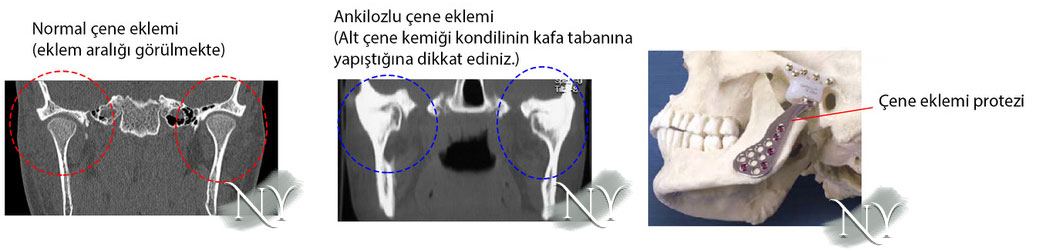 In such a case, it is generally recommended as the first stage treatment to open the adhesion by cutting the bone during surgery, to provide movement to the joint and then to create an artificial joint space by placing materials such as muscle membrane (fascia), tendon, silicone block in between to prevent re-adhesion. This surgery, called gap arthroplasty, is the last exit point before joint prosthesis. However, no matter how well it is done, patients generally require either repeat surgery or treatment with joint prosthesis after 5 years.
In such a case, it is generally recommended as the first stage treatment to open the adhesion by cutting the bone during surgery, to provide movement to the joint and then to create an artificial joint space by placing materials such as muscle membrane (fascia), tendon, silicone block in between to prevent re-adhesion. This surgery, called gap arthroplasty, is the last exit point before joint prosthesis. However, no matter how well it is done, patients generally require either repeat surgery or treatment with joint prosthesis after 5 years.
Joint prosthesis application is the last step of the treatment ladder for jaw joint dysfunction. The number of patients who reach this stage is a very small portion when all jaw joint patients are considered. During the surgery, a larger incision is made and the lateral arms of the mandible bone are removed, including the calcified jaw joint area. This stage requires great care and may cause serious bleeding. Afterwards, the artificial prosthesis suitable for the patient's jaw bone dimensions is fixed to the jaw bone and the temporal bone, which will form the connection at the skull base, using titanium screws. The joint capsule is also repaired. After the prosthesis surgery, the prosthesis may loosen, one or more of the screws may become displaced, and the prosthesis may break. Therefore, patients with jaw joint ankylosis should know that they will not be able to use these joints as if they had never been ill. The results promised by the joint can never be like the person's own natural jaw joint. With the latest technologies, personalized jaw joint prostheses can be produced from three-dimensional printers and mechanically better results can be obtained.