Breast Augmentation Surgery
Everything you need to knowBreast Augmentation Surgery
The ideal candidate for breast augmentation surgery is patients who have sufficient breast skin but insufficient breast volume, who do not have symmetry problems or rib cage abnormalities (such as pigeon chest, shoemaker's chest), who do not smoke, and who do not have internal diseases (such as diabetes, kidney failure). .
Breast enlargement surgeries are among the most commonly performed plastic surgeries, along with liposuction. Patients who only need breast augmentation are generally either young patients under the age of 30 who have never given birth, or patients whose breast tissue, together with the skin, becomes extremely thin after birth, resulting in a small and wizened breast appearance. In both cases, patients must have sufficient breast tissue and skin for augmentation.
Some patients consider the need for breast enlargement and sagging breasts to be the same.
While only breast lift (breast lift, breast lift, mastopexy) surgery can provide satisfactory results for some patients applying for breast augmentation surgery, breast augmentation surgery should be combined in the same session in patients who do not have sufficient breast tissue.
While breast augmentation surgery can generally be performed on women who have completed their development, it can also be performed on younger patients with obvious symmetry differences between the two breasts to prevent psychosocial problems.
The ideal candidate for breast augmentation surgery is patients who have sufficient breast skin but insufficient breast volume, who do not have symmetry problems or rib cage abnormalities (such as pigeon chest, shoemaker's chest), who do not smoke, and who do not have internal diseases (such as diabetes, kidney failure). . In patients with congenital hand and upper extremity, rib cage and pectoral muscle abnormalities, such as the Poland sequence, the breast rather needs to be reconstructed from scratch and multistage treatment is performed ( see Breast reconstruction ).
The normal breast is a structure located between the 2nd and 7th ribs and attached to the rib cage with suspensory ligaments. It has rich blood supply and nervous stimulation.
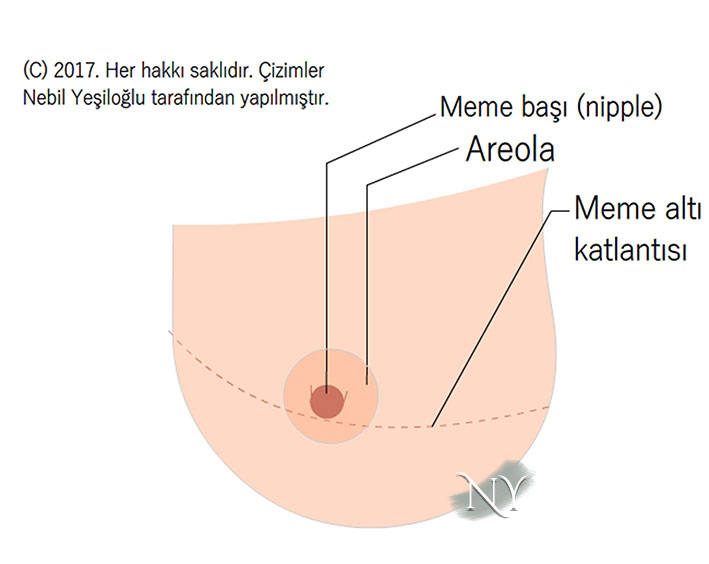
I want my patients who apply for breast augmentation surgery to first learn the most basic anatomical areas of their breasts. Your breast basically consists of the nipple, areola (brown tissue around the nipple), breast tissue, and the submammary fold.
Image Note: In the surface anatomy of the breast, the nipple, areola, breast tissue and submammary fold attract attention.
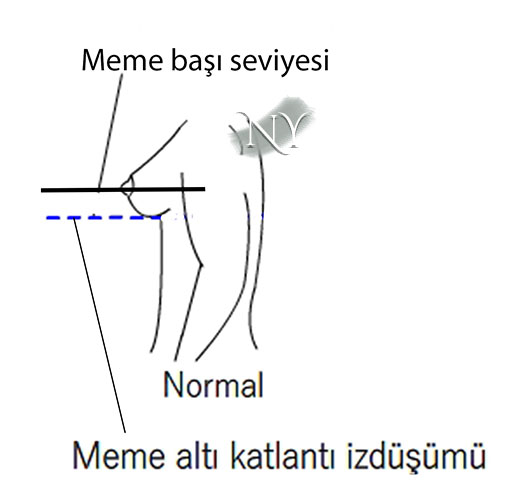
The most basic factors that affect our choice of technique in breast surgeries are the level of the nipple compared to the submammary fold, the width of the breast, the distance of the nipple from the collarbone and the breastbone notch (jugulum).
In a normal breast, the level of the nipple should be at or above the submammary fold (MAK). Breast tissue is also expected not to fall below the MAC.
Visual Note: When viewed from the side, the nipple should be located higher than the peak of the under-breast fold.
Patients applying for breast augmentation surgery must be examined in detail. Among plastic surgeries, breast surgeries require serious questioning and examination.
In patients applying for breast reduction surgery, factors such as the amount of breast tissue, whether it contains cysts, whether there is a history of breast cancer in relatives, and smoking are questioned. After the examination, patients are asked for breast ultrasound if they are under the age of 40, ultrasound and mammography if they are over the age of 40, and if there is any structural mass, it is recorded. This is a resource for post-surgery. When necessary, comparisons are made with new ultrasounds.
Breast augmentation surgery is basically performed by placing silicone prostheses (implants) in the pocket created under the breast tissue on the rib cage. In some patients, additional corrections can be achieved by fat injection to the surface in addition to prosthesis application.
I ask my patients who apply for breast augmentation surgery about the bra size they have used until then and the measurements they requested. First of all, the requested measurement should not strain the rib cage anatomy. Some patients request very large breasts where both breasts meet in the midline like a balloon. Such demands do not make sense for a narrow rib cage.
Silicone prostheses are the factor that provides the results in breast augmentation surgery . Silicone prostheses consist of an outer shell and an inner cavity filled with either integrated gel silicone or saline serum during surgery. Therefore, it is possible to distinguish two basic types: silicone gel prosthesis and saline prosthesis . The patient's demand and the structure of the breast tissue affect the selection.
Image Note: Silicone prostheses are of two basic types according to the material they contain: saline type and silicone gel-containing type.
In saline prostheses, the prosthesis is placed in the empty pocket prepared in the breast and is filled with serum through the tube it contains, and the tube is pulled out.
Breast augmentation surgery does not affect the milk ducts and does not prevent breastfeeding.
It is not expected that lactation function or nipple sensation will be affected in breast enlargement surgeries, especially in patients with submuscular prostheses. Nipple sensation may be affected, although rarely, when inserted around the areola.
I do not recommend surgery to patients until the reduction in breast tissue is clearly established after the lactation process is completed. This is a period of approximately 8-10 months.
The main factor in choosing silicone prostheses in breast augmentation surgeries is the needs of the patient.
Silicone prostheses used in breast augmentation surgeries can be classified according to their various features. For example, there are two main types of prostheses, smooth surfaced and rough surfaced, and a third type, which is covered with an additional shell of spongy polyurethane structure. Those with rough surfaces adhere better to the tissue and are less likely to rotate. It has been reported that they are less likely to cause a problem called capsular contracture around the implant. Dentures with smooth surfaces are easier to place, however, they are more likely to rotate internally. They are less felt by the patient. The rates of developing capsular contracture are slightly higher than those with rough ones.
Image Note: There are two types of silicone prosthesis shell: smooth surface and rough surface.
Silicone prostheses covered with a polyurethane shell are produced considering that the potential of polyurethane to form capsule tissue is less than other types and that the prosthesis adapts better to the surrounding soft tissue. In the first months after placement, the polyurethane shell adapts to the tissue.
Another prosthesis classification can be made according to the shape of the prosthesis. Anatomical (drop-shaped) prosthesis is thinner at the top and thicker at the bottom and gives better results for shaping the breast in patients with thin breast tissue. The round prosthesis has the same thickness at the top and bottom. It shows the fullness of the upper pole better. While it is not a problem for round prostheses to turn upside down, anatomical ones may require surgery if they cannot be corrected with massage.
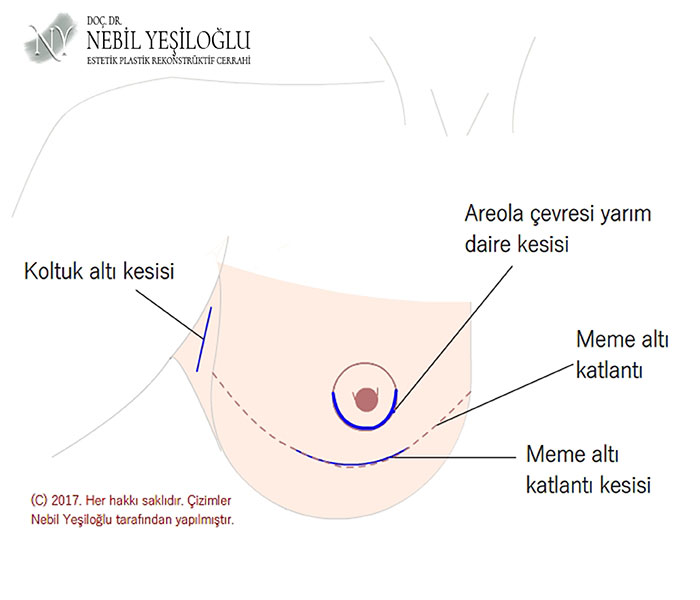
The visibility of the scar left in breast augmentation surgery is related to the patient's choice and skin structure. However, there may be entry points that are not suitable for every prosthesis.
In breast augmentation surgery, the placement points of silicone prostheses are the border of the brown area called areola, the fold under the breast or the armpit.
Image Note: Incision areas used for breast prosthesis placement.
Although recently there are surgeons who place implants through an incision made around the belly button, it is not a widely used technique in practice due to the difficulty of application, unnecessary penetration into the abdominal tissue, and even damage to the sub-breast fold.
In breast augmentation surgery, the incision made in the sub-breast fold varies between 3-6 cm depending on the size of the prosthesis and is hidden in this area.
The incision that can be made around the areola is in the shape of a half moon and is as long as the semicircumference of the areola. It may fade over time and become noticeable depending on the color of the areola. It is not appropriate to use this incision line in patients with a small areola circumference that is below 3cm. If possible, under-breast folds should be used. In incisions around the areola, there is a very low chance that microorganisms from the nipple will infect the implant and cause infection. Another possible problem is that the nerve endings around the nipple may be damaged, causing loss of sensation.
The armpit incision in breast augmentation surgery is generally about 2cm and becomes indistinct in the armpit folds over time. Generally, only saline prostheses are placed through the armpit incision, hollow and rolled up, and inflated while inside. It is difficult to place silicone gel prostheses in such a narrow space. The main disadvantages of the armpit incision are that when they darken, they become visible when wearing sleeveless clothes and they require special equipment for insertion.
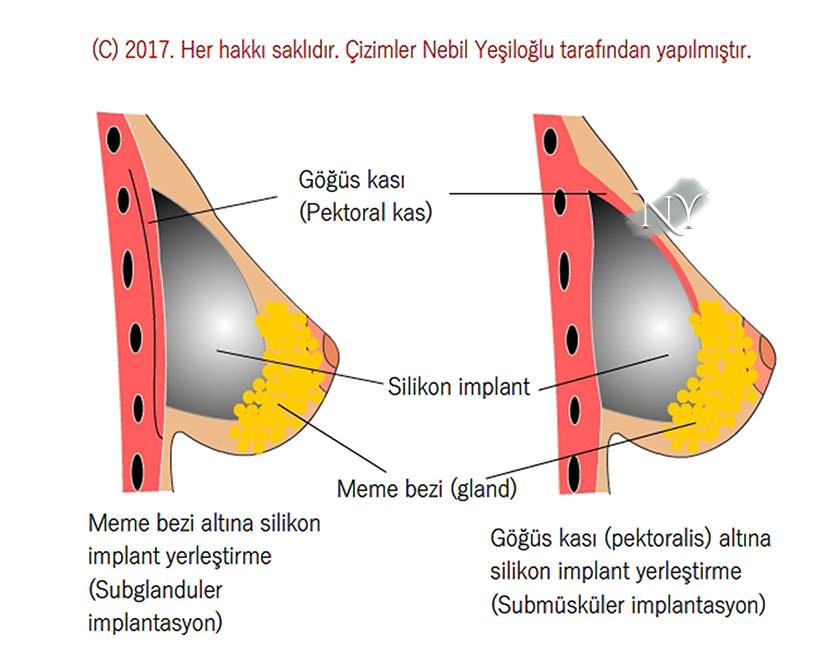
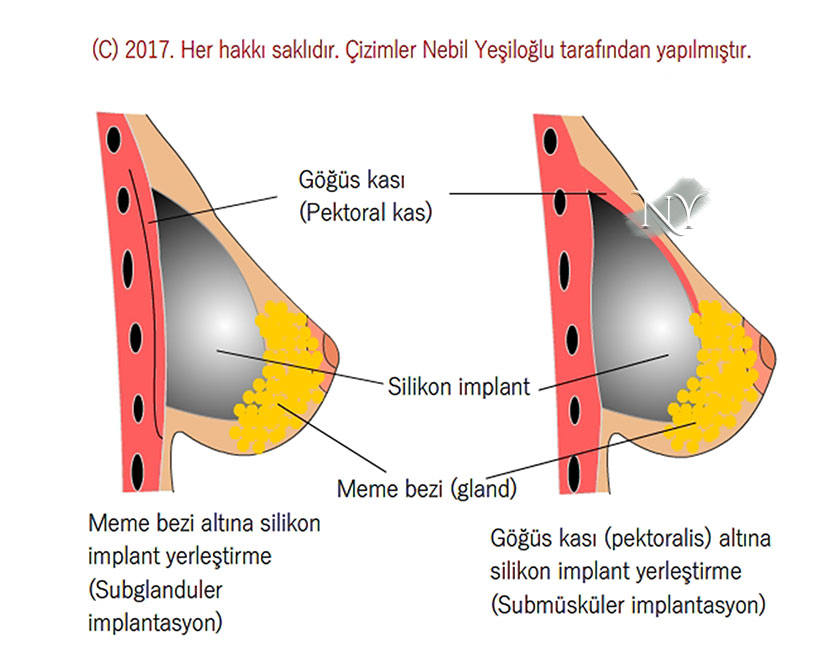
The silicone implant can be placed under the chest muscle (pectoralis major muscle) in the pocket created in the breast or directly under the breast tissue (i.e. above the chest muscle).
One of the most important features that the patient must decide in breast augmentation surgery is the tissue under which the implant will be located. The pectoral muscle provides a nice cover to hide the implant.
Image Note: Placing a silicone prosthesis under the muscle and under the mammary gland
While this cover covers the upper 80% of the implant, the bottom part will still be in contact with the mammary gland. It has been shown that long-term problems (such as pain, capsular contracture) develop less frequently after the implant is placed under the chest muscle . However, in order for the prosthesis to be placed directly under the breast tissue, the breast tissue must be at least 2cm thick. Otherwise, the prosthesis can be easily felt with the hand.
Another advantage of placing a submuscular prosthesis in breast augmentation surgery is that there is no interaction with the breast tissue during the surgery. This provides an advantage in terms of protecting the milk ducts. However, in patients with implants placed under the mammary gland, lactation function is generally not affected.
In breast augmentation surgery , the dual plan prosthesis placement technique is also frequently used to reduce the possibility of the silicone prosthesis getting stuck under the muscle and to provide a more natural transition . For this, the internal connections of the chest muscle are separated. This reduces the likelihood of problems such as double bubble deformity, which can develop especially in patients with a large prosthesis placed in a small pocket.
Image Note: Double bubble deformity in the breast that occurs as a result of compression under the pectoralis major muscle of the chest.
After breast augmentation surgery, you should not smoke and avoid intense activities that will involve excessive movement in the rib cage. In this way, your prosthesis can remain in your body for a longer time without causing any problems.
At the end of breast augmentation surgery, a tube called a drain will be placed in the breast pocket, which is used to collect dirty blood and is usually removed the next day.
Image Note: After breast augmentation surgery, drains coming out of the breast area collect dirty blood.
Apart from this, I recommend you to wear non-wired sports bras suitable for your new breast size for at least 2 months.
In the early period, I recommend that you avoid activities that will strain your chest, such as using a vacuum cleaner, doing pull-ups, or playing tennis, for at least 1 month.
Although surgery-related pain and swelling normally become noticeable in the 3rd month, it may take up to 15 days for the bruises to disappear.
If you are working at a desk job, you can return in two weeks at the latest, but for jobs that require heavy lifting, this is at least 20 days.
I do not recommend starting activities such as swimming before 1 month.
Do not listen to comments such as saying that you will return to your normal life in a few days after breast augmentation surgery.
You can take a shower the day after the surgery. Taking a shower will replace the dressing by cleaning the microorganisms in the body flora. To close the stitch lines on the breast, I recommend applying an antiseptic spray and covering them with gauze for up to 5 days. Afterwards, necessary recommendations will be made during the checks. I recommend that your stitch lines be protected with sunscreen, even if you are wearing clothes, for at least 7-8 months. The stitches placed during the surgery are located under the skin and do not need to be removed, and there is no scar caused by the stitches. I recommend special gels for patients with swollen wound healing problems in their early follow-up visits.
Negative consequences (complications) that may occur after breast augmentation surgeries should be evaluated as early and late.
Pain formation in the first days after surgery is natural and requires good painkiller support. This situation is observed more frequently, especially after submuscular prosthesis applications.
Early problems that can be observed after breast augmentation surgery are as follows;
- Collection of blood or fluid in the breast pocket (may require taking into the operating room
- wound line infection
- Prosthetic pocket infection (requires removal of the prosthesis in the operating room, cleaning of the pocket, and readmission to the hospital.
- Surgery-related edema and swelling in the breast that regress over time (this swelling may be asymmetrical and prominent in the upper pole.)
- Especially in patients who need to readjust the under-breast fold, the prosthesis may slide downwards.
The most important problem encountered in the late period after breast augmentation surgery is the formation of capsular contracture , which is characterized by tensions and deformities in the connective tissue capsule formed by the body around the prosthesis .
Image Note: Removed breast prosthesis and surrounding capsule tissue.
The capsule begins to form around all dentures from the 3rd month onwards and contributes to the strengthening of the prosthesis. However, capsular contracture is not observed in every patient. It is painful and you should decide together with your doctor during the examination regarding follow-up or implant replacement. When capsular contracture occurs, the basic treatment is surgical removal of the capsule (partially or completely) and the prosthesis followed by the placement of a new prosthesis.
A problem that can be seen in the late period in the patient who has an implant placed under the armpit is the implant shifting upwards and outwards. This is caused by the soft tissue at the outer border of the breast having to be opened during surgery.
Capsule contracture is a reaction of the connective tissue to the prosthesis. Although many factors have been blamed, such as small blood accumulation in the prosthesis pocket, subclinical infections around the prosthesis, and the powder of the gloves used in surgery, the exact cause is not clear.
Although many experimental and clinical studies have been conducted to regulate both prosthetic technologies and patient-based factors to prevent capsular contracture that may occur after breast augmentation surgery, there is no method, drug or solution that is fully established in the clinic. However, the basic recommendations for prevention include placing the prosthesis under the muscle, using powder-free gloves, and using prostheses with rough surfaces.
Breast implants are covered with a very durable shell and are unlikely to be injured unless approached with a piercing or cutting tool.
The prostheses used in breast augmentation surgery are subjected to very detailed mechanical tests. They are not expected to tear unless an object that causes puncture is pricked. A patient of mine asked me if it would explode due to the pressure difference when he got on a plane. You can be sure that it is not produced with a technology that produces such poor results. Although manufacturers generally give a period of 15 years for the lifespan of prostheses, I recommend my patients to replace their prostheses after 10 years.
There is no scientific evidence that the prostheses used in breast augmentation surgeries cause breast cancer. However, recently a very benign mass known as anaplastic cell lymphoma (ALCL) has been described, which was found to develop from the capsule tissue approximately once in 300 thousand.
In long-term analyzes of the capsule tissue in breast augmentation surgeries, especially in the statements made by international and national plastic surgery associations, it has been stated that an intermediate level tumor associated with lymphoma of the lymphatic system may develop in the capsule tissue. However, prospective studies are still ongoing to determine whether this is directly related to the implant. Although the fact that these rare cases have been encountered while the quality is gradually increasing in the production lines of companies has created a prejudice against breast augmentation surgeries, the mentioned lymphoma-like tumor can be easily treated by completely removing the implant and capsule tissue. It does not require radiotherapy (radiation therapy) or chemotherapy (treatment with cancer drugs). Regarding this issue, you can access the informational article of the Turkish Plastic Reconstructive and Aesthetic Surgery Association, which is the most competent organization in the field of plastic reconstructive and aesthetic surgery in our country, by clicking here .
It is not true that breast cancer screenings will be interrupted after breast augmentation surgery.
No disruptions in breast scans are expected after breast augmentation surgery. However, in examinations such as mammography, this may be difficult because the breast tissue must be pressed to the ground. However, in patients who have undergone breast augmentation surgery, breast ultrasound and, if necessary, MRI (magnetic resonance) examination of the breast provide sufficient detail. Apart from this, I recommend breast ultrasound in the preoperative period and mammography for those over the age of 40. On the other hand, in a comparative and very valuable study conducted on 260 breast cancer patients, no statistically significant difference was found in terms of the stage of cancer when diagnosed with breast augmentation surgery and patients without augmentation (1) . This shows that there is no problem in breast cancer screenings. On the other hand, another result of this study is that in patients with subglandular breast prostheses placed directly under the breast tissue, the frequency of detecting a noticeable tumor only during manual examination, compared to the prostheses placed under the chest muscle, is in the first group. was found to be higher. Patients who have a prosthesis placed under the mammary gland should be more sensitive during follow-up. Since there is no relationship with the breast tissue in patients with a prosthesis placed under the chest muscle, it is unlikely that there will be any confusion or disruption in the follow-up of the patients.
Source:
- Cho EH, Shammas RL, Phillips BT, Greenup RA, Hwang ES, Hollenbeck ST. Breast Cancer after Augmentation: Oncologic and Reconstructive Considerations among Women Undergoing Mastectomy. Plast Reconstr Surg. 2017 Jun;139(6):1240e-1249e.
"Health is the most important thing you have in life!"
Contact us now to schedule an appointment.