Breast Reduction Surgery
Everything you need to knowBreast Reduction Surgery
The critical point in choosing the surgical technique in breast reduction surgery is the location of the normal location of the nipple and areola relative to the location available in the patient.
Breast reduction surgery is one of the most preferred surgeries in our country, at least as much as breast augmentation surgery. As well as being an organ of self, the breast has also played a status determining role in societies for centuries. In old historical artifacts and painting motifs, the female breast is depicted as large, symbolizing fertility.

Image Note: In the Kybele statue found in the Çatalhöyük excavation, breasts are depicted as large.
However, the weight of the breast becomes more disturbing over time and patients want to get rid of the size of their breasts.
Breast reduction surgery may leave visible scars on the breast, but patients demand a reduction in the burden as well as fewer scars.
Although breast size is mainly affected by genetic factors (inherited characteristics), in some women, the decrease in breast volume after the breastfeeding period is much lower than expected, and therefore large breasts begin to bother after a while.
Large breast weight and volume negatively affects spine and shoulder health (1). There is no clear defining characteristic of the upper limit of breast size because inter-racial and inter-individual sizes can vary significantly. The definition of large breasts in a tall woman with a narrow rib cage is different from the definition of a short woman with a wide rib cage. In my personal opinion, breast size that affects the biomechanics of the shoulders and spine and causes pain in these areas can be considered large. The most obvious effect of the trauma caused by the breast on the shoulder is the scar and hump left by the bra strap.
Breast reduction surgery can be performed starting from the age of 15, when the breast has completed its development in adolescence (2). Dimensions that negatively affect the social life and daily activities of the patient under the age of 18 should be evaluated together with the family in terms of surgery.
Before breast reduction surgery, I would like to evaluate a detailed breast examination, breast ultrasound and, for those over the age of 40, tests called basal mammography, which should always be maintained.
Breast reduction surgery can actually be considered the most important diagnostic method for a possible breast cancer diagnosis, as it involves removing tissue from the breast. The parts taken during breast reduction surgery are marked during the surgery and sent for pathological examination, and if any cancer focus is detected, relevant treatments and breast reconstruction surgery can be applied.
The critical point in choosing the surgical technique in breast reduction surgery is the location of the normal location of the nipple and areola relative to the location available in the patient.
Breast reduction surgery requires moving the areola and nipple to their normal position in the breast.
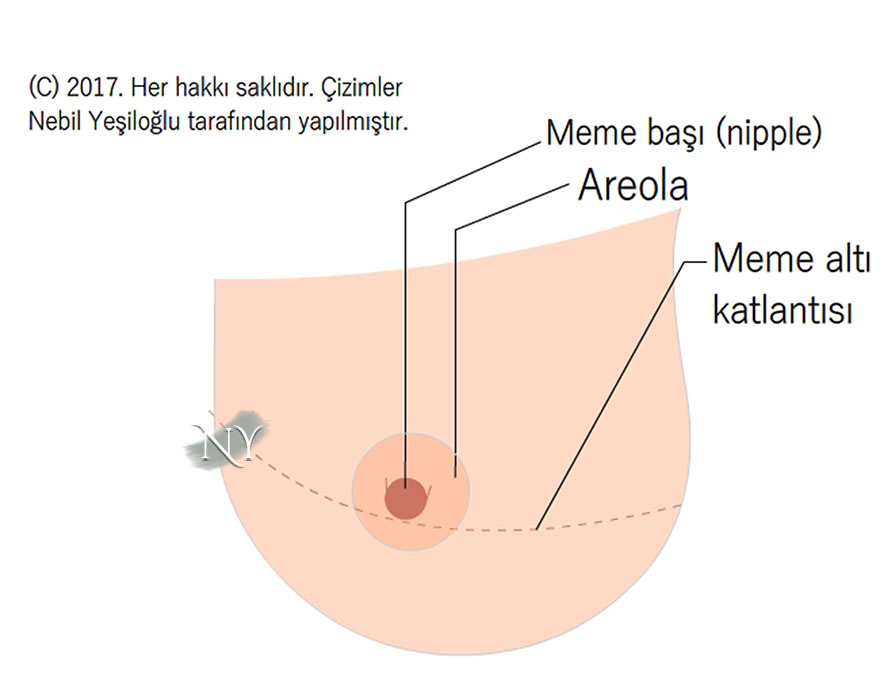
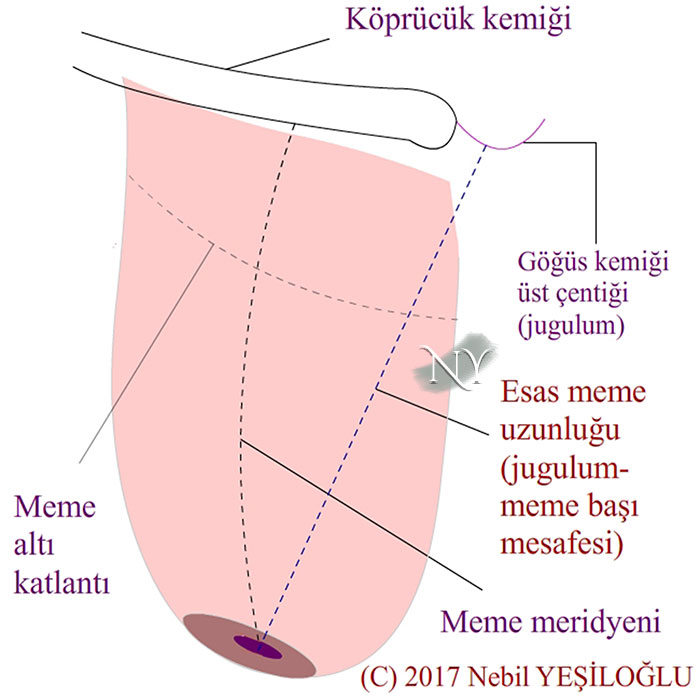
Image Note: Surface anatomy of the normal breast
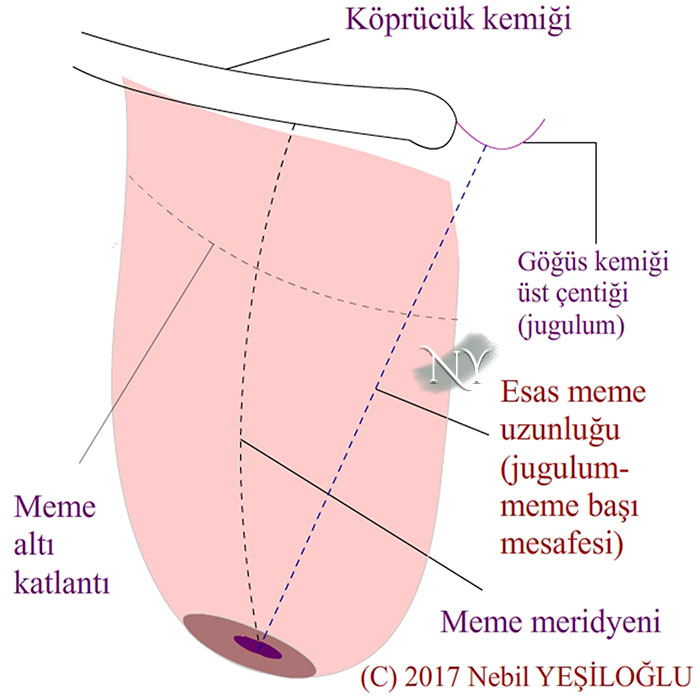
For this purpose, various measurements should be made on the breast. The most important of these is the distance of the nipple to the collarbone and the breastbone notch (jugulum).
Image Note: Important measurements made in breast reduction surgery.
This distance is approximately 21-22 cm on average. However, as I mentioned before, personal norms may vary and each patient is evaluated on his or her own merits.
The main goal in breast reduction surgery is to move the areola and nipple slightly above the level of the submammary fold, as in breast lift surgery.
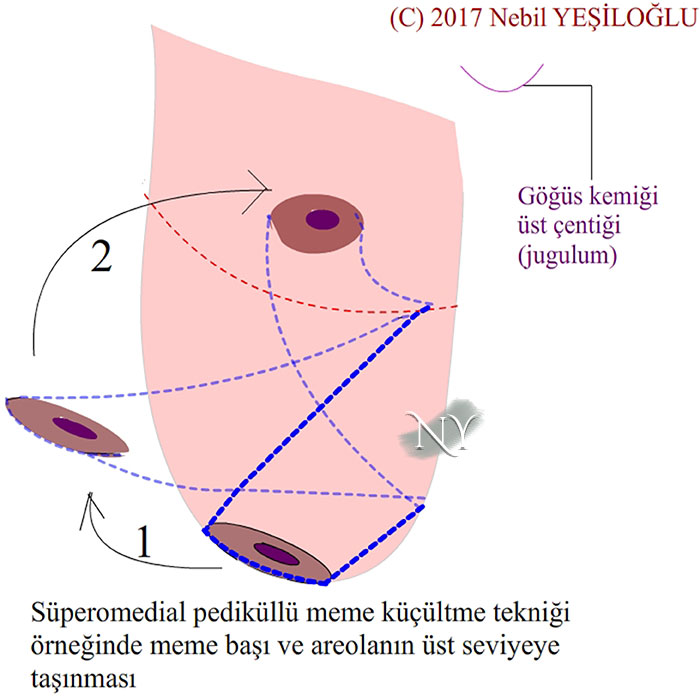
In breast reduction surgery, tissue bridges called pedicles are used to transport the nipple and areola. While these bridges are connected to the body at one end, the other ends are free and carry the nipple and areola.
The basic step in breast reduction surgery is moving the nipple and areola. The remaining tissue is shaped within the framework of this transport. As I mentioned, when the nipple-sternum notch distance exceeds 21-22 cm, it is necessary to move the nipple and areola with tissue bridges in a way that does not disrupt the blood circulation and sensation in order to reach these measurements.
Image Note: In the example of breast reduction surgery with the upper pedicle technique, the nipple and areola are moved to the required level through the pedicle tissue.
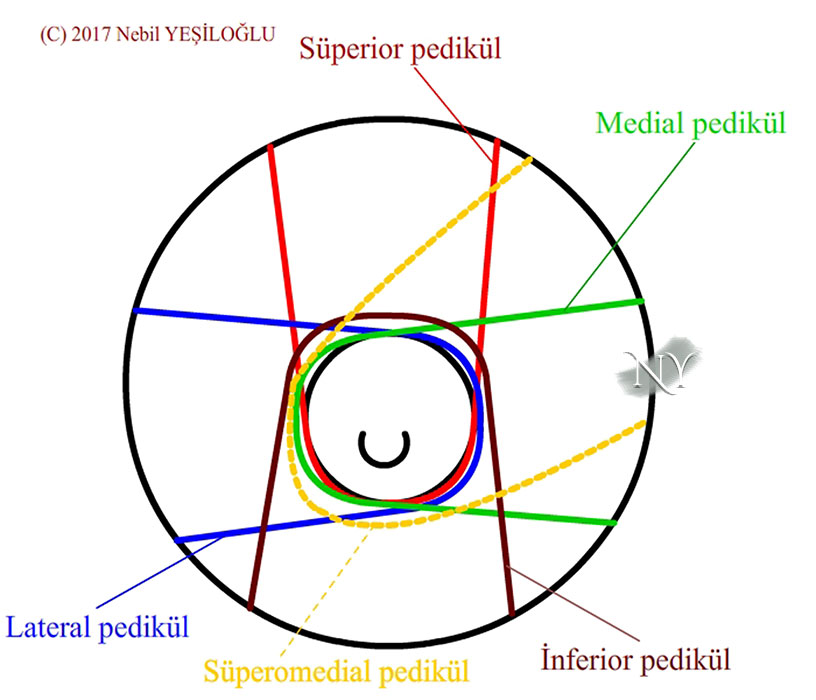
These bridges, called pedicles, are prepared with critical width and length ratios in plastic surgery. When these rates are exceeded, the blood supply to the nipple and areola may be impaired and may be lost. Various pedicle types have been defined according to the point at which the pedicle tissue sits at the base. Depending on the area where they attach to the breast, external (lateral), internal (medial), upper (superior), lower (inferior) and central (central) pedicle techniques and their variants are the main pedicle creation techniques used.
Image Note: Various pedicle preparation methods.
As we said, the determining factor here is the possible pedicle dimensions.
In breast reduction surgery, the possibility of blood circulation deterioration increases with pedicle sizes exceeding 34-35 cm, and in this case, breast shaping will become difficult. In these patients, the nipple and areola are removed at the beginning of the surgery, like a button, and kept in a serum-soaked gauze, and at the end of the surgery, their ideal location is determined and adapted again. In this method, defined as free nipple graft technique , it is not possible to feel the nipple and areola in the future. Again, it is not possible to give milk with this technique. On the other hand, in the later period, there may be discolouration in the adapted nipple and areola tissues.
There are also techniques that can be tried in patients whose breast length (nipple-breast notch distance) is above critical values but who want to be able to breastfeed and feel the nipple in the future. However, adequate reduction may not be achieved in these patients.
Especially in young women who have not had children, the choice of technique to protect the nipple and milk ducts is a must. However, exceeding the critical length in these techniques may still lead to nipple and areola loss. I talk about this in detail with my patients. Another situation is that the breast tissue will not shrink sufficiently. In these patients, the prepared pedicle will create volume in the breast on its own.
The scars that will remain after breast reduction surgery are related to the volume of the breast and excess skin.
Breast reduction surgery is performed under general anesthesia, that is, with the patient asleep, and takes between 2-4 hours. Although the average wound healing process is 15 days, I recommend that patients avoid activities that strain the rib cage before the end of the first month (tennis, swimming, using a broom, etc.). Sometimes, it can take much longer for the breast to heal, especially in patients with fibrocystic breasts identified on breast ultrasound. In these patients, dissolving breast tissue may be discharged from the suture lines in the form of a transparent discharge. These complaints will regress with regular dressing. Very rarely, it may be necessary to repair it with stitches a second time.
After breast reduction surgery, tubes called drains are placed to remove dirty blood that may accumulate inside. These are removed on the third day of surgery at the latest.
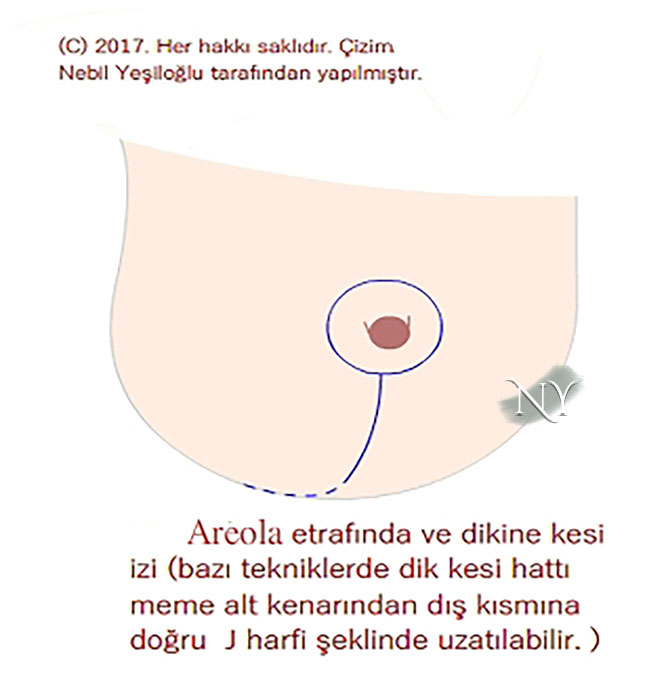
Depending on the rate of breast reduction after surgery, the scar that will remain may remain in the shape of a lollipop (breast reduction with vertical scars) or its extended J-shaped form.
Image Note: Surgery scar in the shape of the letter J. The slightly shorter one ends at the sub-breast fold and is defined as a vertical scar (vertical scar mammoplasty).
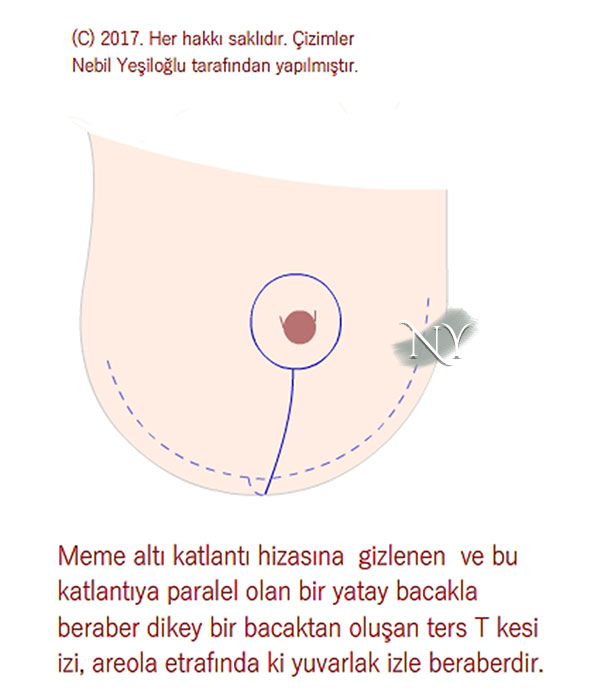
In larger breasts, it may be necessary to leave a scar in the shape of an inverted letter T by extending the scar along the sub-breast fold in order to tighten the skin in the horizontal axis.
Image Note: Breast reduction surgery ending with a scar in the shape of an inverted T letter.
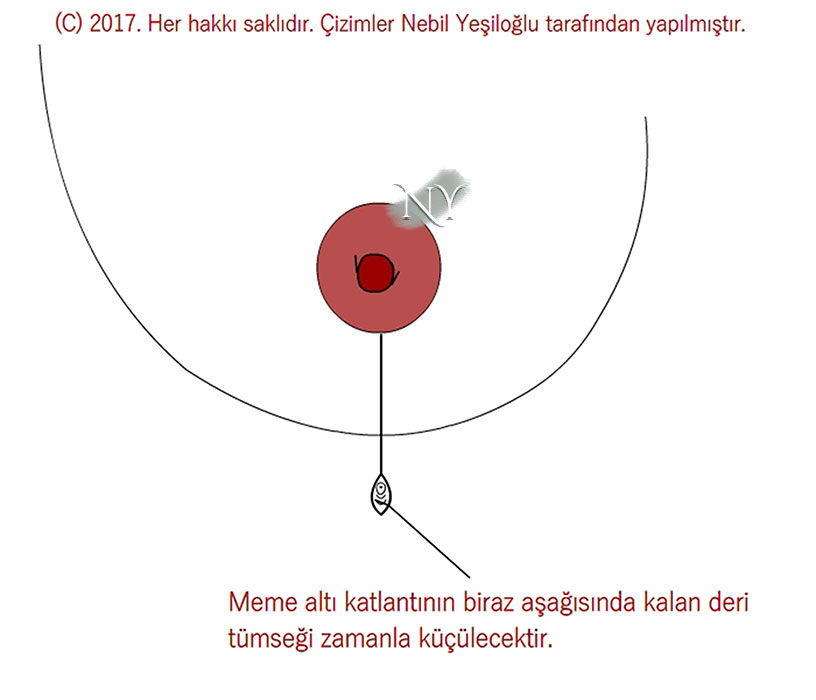
In breast reductions with vertical scars, a tissue bump may remain at the lower end of the scar.
Image Note: Tissue bump that may remain in vertical scar breast reduction.
This bump may be necessary to prevent the scar from turning into an inverted T, and it usually disappears within 1-3 months.
I have patients who apply to have their breasts reduced using the liposuction technique. In breast reduction surgery, the liposuction technique is used to eliminate surface irregularities that may remain on the surface of the breast.
Breast reduction surgery can be performed in combination with liposuction (fat removal) technique. Our main goal is to eliminate any additional excess and surface irregularities that may remain in these patients, especially on the outside. Using the liposuction technique alone for breast reduction will only leave behind an empty, sagging and wilted breast sheath.
Unlike the liposuction technique in breast reduction surgeries, fat injection is one of the techniques used to shape the breast surface, although less frequently. Here, some volume can be provided by fat injection, especially in patients with insufficient upper pole fullness. However, when the injected volume is above a certain amount, fatty cysts or calcium precipitates into the injected fat and calcification may occur. In this last case, the resulting mass may need to be removed.
Breast reduction surgeries are the largest plastic surgeries performed on the breast. Various problems may arise in the early and late periods after the surgery, and some of these are problems that could not be predicted before the surgery.
Problems that may arise in the early stages of breast reduction surgery, related to the breast itself, can be listed as follows;
- Accumulation of blood (hematoma) or fluid (seroma) within the breast tissue despite drainage.
- Breast wound line or breast tissue infection
- seam separation
- Asymmetry in the breasts and obtaining results below the expected result.
- Tissue losses in the nipple and areola
- Loss of sensation in the nipple and areola (this is already expected in the free nipple carrier technique)
Many of these problems can be resolved in collaboration with your surgeon. Some problems may require return to the operating room.
Late-term breast problems that may occur after breast reduction surgery are mainly as follows;
- Prominent (raised) scarring; In some people, it is associated with the body's excessive response to wound healing and is alleviated with some injections and silicone layer applications. In some patients, scars may widen along with weight gain.
- Shifting of breast tissue towards the lower pole of the breast (bottom out deformity) is a condition that may occur in all surgical techniques due to reasons such as gravity, advancing age or pregnancy. If it is advanced, it may require surgical correction. This problem is more common in inverted T-shaped surgical scars. Be sure to keep your weight balanced after breast reduction surgery. Weight gain can lead to significant changes and reversals in breast shape.
- Changes in nipple and areola color are a problem we usually observe in the free nipple handling technique, but can also be observed in other techniques. Any trauma applied to these tissues, which are brown to pink in color, can create such a result. Your doctor will suggest solutions to these problems.
The relationship between breast reduction and pregnancy and lactation are important issues that my patients are curious about.
Breast reduction surgeries other than the free nipple carrying technique generally do not negatively affect lactation functions. However, this possibility is not excluded. Although it is unlikely, lactation function may be negatively affected in patients. However, there are also broad-based publications indicating that lactation function is not affected (3).
I do not recommend getting pregnant until at least 1 year after breast reduction surgery. This is necessary to complete the process of shaping the shape of the breast. Likewise, I recommend that the breast be reduced at the earliest in the first year after the breastfeeding process ends. Because the effects of breastfeeding do not go away in 2-3 months. This waiting period is necessary especially to prevent the milk ducts from shrinking and thus being damaged.
The idea that breast reduction surgery hinders the monitoring of the breast for cancer is erroneous and not based on scientific evidence.
Breast reduction surgeries have also become among the auxiliary techniques used in breast cancer surgeries. Especially after the removal of cancerous tissue with limited surgery (such as lumpectomy), the breast can be shaped with breast reduction techniques by selecting the pedicle according to the area where the loss occurs in order to provide a repair without creating deformity in the breast. This is called oncloplastic breast surgery. Again, for limited cancer foci, the removal of cancer can be performed like a breast reduction procedure, ensuring that the breast remains in a more anatomical shape. On the other hand, the tissue pieces obtained in breast reduction surgery can be subjected to direct pathological examination and a diagnosis of breast cancer can be made without leaving any room for doubt. I have detected such cases of breast cancer in a few of my patients.
Breast reduction surgery is also successfully performed in unilateral breast asymmetries or in eliminating the disproportion with the opposite breast in a patient who has received breast cancer treatment for which a new breast is created.
Before breast reduction surgery, breast screening tests and breast examination, as I mentioned at the beginning, are important in identifying previously existing breast masses. The presence of masses other than these should be evaluated in subsequent imaging tests.
Resources:
- Nicoletti G, Passaro I, Malovini A, Faga A, Toffola ED. Objective integrated assessment of functional outcomes in reduction mammaplasty. Plast Reconstr Surg Glob Open. 2013 Nov 7;1(7):e61.
- Nuzzi LC, Firriolo JM, Pike CM, Cerrato FE, Webb ML, Faulkner HR, DiVasta AD, Labow BI. The Effect of Reduction Mammaplasty on Quality of Life in Adolescents With Macromastia.Pediatrics. 2017 Oct 6. pii: e20171103.
- Thibaudeau S, Sinno H, Williams B. The effects of breast reduction on successful breastfeeding: a systematic review. J Plast Reconstr Aesthet Surg. 2010 Oct;63(10):1688-93.
"Health is the most important thing you have in life!"
Contact us now to schedule an appointment.